Blood Typing

BACKGROUND:
Blood Types: The fundamental function and composition of blood is the same in everybody. However, there are several blood types within the human population, and they are not compatible with one another when it comes to blood transfusions. This variation in blood types results from differences in red blood cell surface molecules. Like other cells, there are molecules that project from the surface of the cell membrane of red blood cells. Some select sugar and protein molecules on the surface of the cell act as identification markers that indicate the cell is a normal part of the body; and therefore, the immune system knows not to attack it. If blood from an individual with different surface molecules is transfused into another, the immune system recognises it as antigenic (foreign to the body) and therefore attacks the Antigens in an attempt and the cells that carry them. To combat this, donated blood is tested for A, B, O, and Rh Antigens, so that blood is only transfused into compatible recipients.
The ABO Blood Groups: The presence or absence of two Antigens, A and B, on the surface of the red blood cells result in the ABO blood groups (types). The immune system recognises Antigens that are present very early in life as a normal part of the human body, and therefore does not develop an immune response to them. Antigens are inherited from the parents’ genes. Without an immune response, antibodies to any A and B Antigens present in the blood cells are not developed in the body. However, A and B blood Antigens not present on the organism’s own cells will cause the immune system to produce antibodies. In blood Type A, the A antigen is present on its red blood cells and anti-B antibodies are present in the Plasma. In blood Type B, the B antigen is present on its red blood cells and A antibodies are present in the Plasma. Type AB blood contains both A and B Antigens on the red blood cells and no antibodies are present in the Plasma.
Type O blood contains neither A or B Antigens on the red blood cells and both A and B antibodies are present in the Plasma. These antibodies will be present, regardless of whether the person has had foreign blood introduced into their body. The antibodies are believed to be present due to the similarity between A and B blood Antigens and common Antigens we encounter in the environment. Antibodies generated for one antigen will recognise another if the two Antigens are very similar.
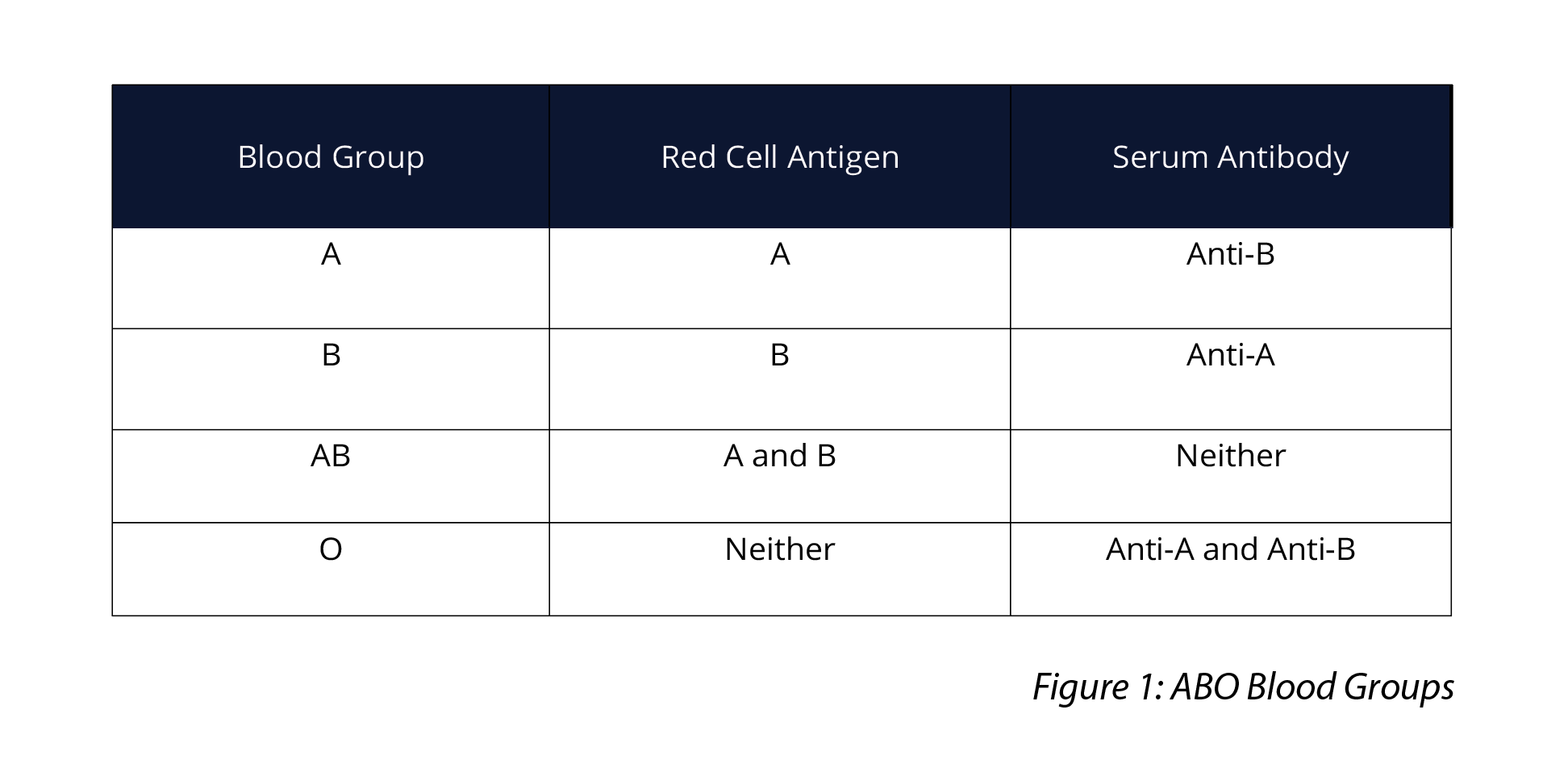
Figure 1: ABO Blood Groups
The Rh Blood Groups: The Rh antigen refers to a group of closely related Antigens. Rh positive (Rh+) refers to blood that contains an Rh antigen. Blood that does not contain the Rh antigen is Rh negative (Rh–). Rh antibodies are only produced if the individual has had prior exposure to the antigen, such as would occur in an Rh– pregnant woman carrying a foetus that was Rh+.
Using Agglutination to Determine the Blood Type: Agglutination describes the clumping of particles and results from an antigen being mixed with its corresponding antibody. For example, agglutination will occur in a blood test if blood type A interacts with Anti-A antibody serum.
In this investigation, students are tasked with determining an unknown blood type in a sample of synthetic blood using the presence or absence of agglutination as evidence. This involves adding a single drop of blood into each of the wells on a blood typing slide, labelled A, B, and Rh. Students add a drop of each synthetic antibody serum to the corresponding well. Once the serums have been mixed into the blood sample, students will observe the presence or absence of agglutination in each well to determine which of the antibody serums (Anti-A, Anti-B or Anti-D) the blood reacted to. Blood type is determined by identifying with antibody serum the blood reacted with. Students repeat this procedure three more times to determine the ABO and Rh blood types of four samples.
METHOD - STUDENT ACTIVITY
-
Collect your blood typing slide and examine it. You will observe that the slide contains three wells, labelled A, B and Rh.
- Collect sample 1 and add one drop of the synthetic blood sample to each well using the dropper vial. Replace the cap on the vial to prevent cross-contamination between different samples. Ensure you replace the lid each time before opening a new vial.
- Add a single drop of each synthetic antibody serum to the appropriate well as follows:
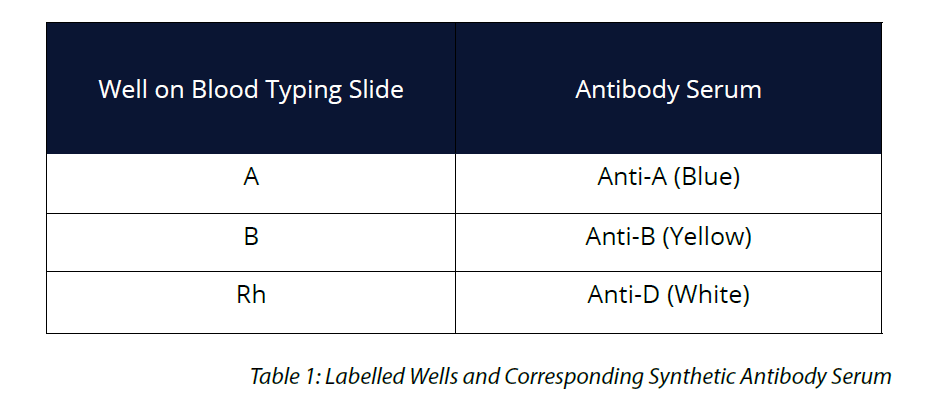
-
Using a mixing stick, carefully mix the synthetic blood and antibody serums for 30 seconds. Use a different mixing stick for each sample to avoid cross-contamination. Use a blue mixing stick for anti-A, yellow for anti-B and white for anti-Rh.
- Once all the serums have been mixed into the synthetic blood sample, examine the samples in each well and look for the presence or absence of agglutination. If the liquid has a uniform texture, no agglutination has taken place. A granular sample will indicate that agglutination has taken place.
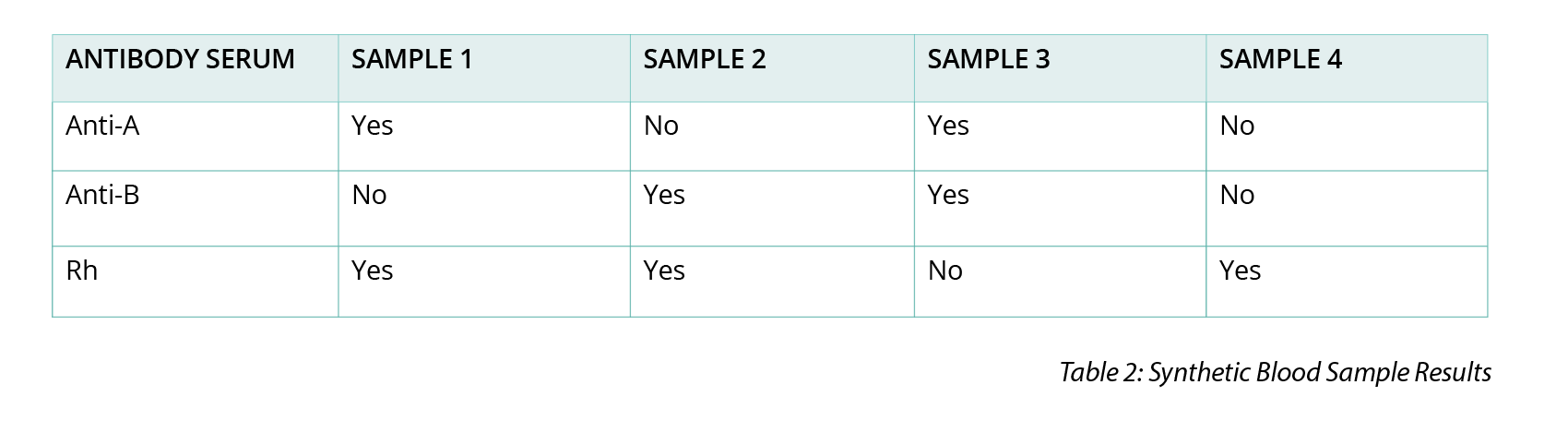
- Record your results in Table 2 in the ‘Sample 1’ column. Simply write ‘yes’ or ‘no’ as to whether agglutination occurred with each antibody serum.
- Rinse the blood typing slide thoroughly over the sink, using tap water. Dry with a paper towel.
- Repeat the same procedure (steps 2–7) using synthetic blood samples 2, 3 and 4.
- Once you have your results for each synthetic blood sample, use the results in Table 2 to determine the blood type of each sample. Remember, a reaction (agglutination), indicates that the synthetic blood sample contains the corresponding antigen to the antibody serum. Record your results in Table 3.
OBSERVATION AND RESULTS

INVESTIGATIONS
Ask students to complete the following activities:-
A break-in occurred at Harold’s jewellery store on Friday night. The thief smashed all the windows open and ran off with $20,000 worth of jewels. However, the thief also cut themselves on some broken glass in their rush to escape the fast approaching police. The forensic team collected some of the thief’s blood that was left behind on a shard of broken glass. After conducting blood tests, the forensic team was able to determine the blood is O–. A witness saw somebody running away from the jewellery store shortly after the crime was committed and provided police with a description of their appearance. The police then brought in a suspect matching the description and noticed a cut on their leg. The police collected a sample of the suspect’s blood to test for blood type. The suspect's blood is mixed with anti-A serum and the test results clearly show the suspect’s blood is not the same as the blood found at the scene of the crime. How did the test results indicate that the blood at the crime scene did not come from this individual?
- The suspect’s blood must have agglutinated in the presence of anti-A serum, indicating that this blood is A-type, and therefore not the same as the blood left at the scene.
- Imagine another suspect was tested with anti-A or anti-B and their blood did not agglutinate, but when tested with anti-Rh it does. Does this information mean the blood left at the crime belongs to this suspect? Explain your answer.
- This suspect has O-type blood, but the anti-Rh serum results show that it is O+, and therefore not the guilty person.
- Jeff and Kim are first time donors taking part in a Red Cross blood drive. Before they can donate, their blood needs to be typed. Jeff is A+. Kim is AB+.
- Identify which ABO antibody/s are present in Jeff’s blood.
- Jeff has anti-B antibodies
- Identify which ABO antigen/s are present in Kim’s blood.
- Kim has A, B and Rh antigens.
- Both Jeff and Kim’s donated blood is sent to be processed and in both samples the blood cells are separated from the plasma. The separated cells and Plasmas are then to be used in blood transfusions. But a blood researcher wishes to extract identify the A antigen in Jeff’s blood. Should the researcher attempt to extract the A antigen from his blood cells or his plasma?
- The A-antigen is part of the membrane of blood cells, so the researcher should use the red blood cells.
 Time Requirements
Time Requirements
- 45 mins
 Material List
Material List
- 1 Vial of Sample 1 Synthetic blood
- 1 Vial of Sample 2 Synthetic blood
- 1 Vial of Sample 3 Synthetic blood
- 1 Vial of Sample 4 Synthetic blood
- 1 Vial Synthetic anti-D (anti Rh) Serum
- 1 Vial Synthetic anti-A Serum
- 1 Vial Synthetic anti-B Serum
- 4 Blood Tiles
- 4 Blue Mixing Sticks
- 4 Yellow Mixing Sticks
- 4 White Mixing Sticks
- 5 Plastic Pipettes
- Paper Towels
- Disposable gloves
- Access to Tap Water and a Sink
 Safety Requirements
Safety Requirements
- Simulated blood will stain skin and clothing. Avoid any direct contact with skin and clothing and wear appropriate PPE, such as gloves and lab coat.
- Know and follow all regulatory guidelines for the disposal of laboratory wastes.